Table of Contents
Imagine walking into a clinic where the clinician checks your neck movement and then schedules a follow-up appointment for the next week. When you return, a different clinician performs the same test. However, this time, the results differ. Although the patient hasn’t changed, the numbers do. You might see this discrepancy as insignificant, but such a small inconsistency can alter the entire case.
In this blog, we will discuss the importance of standardizing cervical range of motion testing and why it is essential for ensuring reliable clinical outcomes. Let’s get started.
Testing variation that alters the clinical picture
When clinicians use their own techniques, the outcomes can vary significantly. For example, one clinician might place their hand slightly higher on the patient’s head, while another supports the shoulder differently. Some clinicians may rush through the cues, while others take their time. Although these differences may seem minor, each one can influence the results by a small margin.
The comfort level of the patient also affects the outcomes. Some patients push until they feel a mild stretch, while others stop when they experience tension. When these variables are combined, they create a confusing set of measurements that may appear valid but do not accurately reflect the patient’s true mobility.
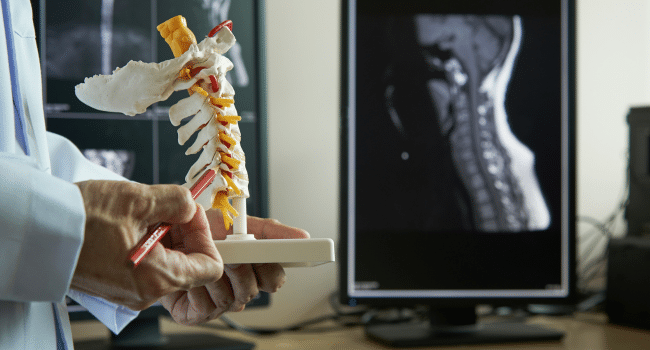
Using tools for cervical joint position error tests can make diagnoses easier and more precise. These tools follow a consistent pattern that is stricter than what human clinicians typically do.
How small inconsistencies turn into wrong conclusions
Here’s a situation: a clinician reports that a patient has gained eight degrees of rotation, while a co-worker notes a decline in the same measure. Neither scenario indicates true improvement or deterioration; it simply highlights how easily test results can vary when different methods are used.
This variability can impact subsequent decisions. For example, a therapist might increase exercise intensity because the chart seems to show positive progress, or reduce manual therapy based on readings that suggest improvement. In reality, these changes may simply reflect differences in how the tests were conducted.
Why accurate diagnosis depends on stable testing
Neck disorders often present with similar symptoms. Muscle guarding can resemble joint irritation, while facet issues may mimic disc problems. Subtle differences in rotation, side bending, or extension can help distinguish these conditions, but this is only effective when the measurements are consistent.
If the testing method changes from session to session, these patterns can become blurred. A condition that requires precise mobility thresholds becomes increasingly difficult to identify. Rather than narrowing down the possibilities, the clinician is left working with distorted clues.
The diagnosis improves significantly when the raw data is clear. Clean data is achieved through standardized testing.
How standardization guides treatment choices
Treatment planning relies on recognizing patterns in patient progress, including where mobility begins to improve, where it stalls, and how the patient responds over time. A structured testing protocol helps to keep these trends visible. This allows the clinician to know when to introduce rotation drills, when to add loading, and when to hold back.
Without standardization, it becomes challenging to identify what is effective and what is not. For instance, one session might show progress simply because the head was aligned differently, while another session might obscure progress due to the clinician positioning themselves at a different angle.
Establishing clear protocols creates a stable baseline for evaluation. A stable baseline makes treatment planning more reliable.
How instruments strengthen the entire process
Clinicians often rely on their eyes and hands to assess patients. While experience is valuable, even skilled observation has its limitations. Small movements can be difficult to judge accurately, and factors such as fatigue, bias, or established habits can affect a clinician’s perception.
This is where instrument-based testing comes in to provide clarity when human observation is uncertain. A cervical range of motion instrument offers consistent readings that are unaffected by mood, fatigue, or interpretation. It delivers the same measurement for the same movement every time.
It’s important to note that this does not replace clinical reasoning; rather, it supports it. The clinician can still evaluate the quality of motion, observe patient behavior, and respond to symptoms while the instrument takes care of the numerical data.
How consistent data improves clinic-level performance
Even small clinics benefit from internal data tracking. Over time, patterns appear. Some treatments show stronger results. Some patient groups respond quicker. Some clinicians record faster improvements.
These insights depend on reliable data. Without standardized testing, numbers from one provider cannot be compared to those from another.
When cervical ROM testing follows the same protocol across sessions and providers, the data turns into something meaningful. Clinics can audit results, compare treatment approaches, and refine what they offer.
Conclusion
Cervical range of motion testing may seem straightforward, but its significance is profound. When the testing method changes, the results can change as well. These changes in results can alter the entire clinical narrative. Standardizing this testing process ensures accuracy, enhances diagnoses, improves treatment planning, and leads to more reliable long-term outcomes.
By using consistent protocols and objective instruments, clinicians gain better clarity, allowing them to provide care that accurately reflects the patient’s true condition. This standardization makes the entire clinical process smoother, more consistent, and more trustworthy.