Table of Contents
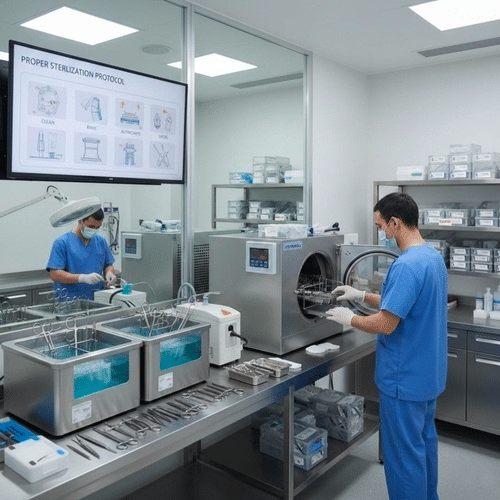
Proper sterilization and renovation of surgical gadgets are vital to ensuring affected character protection, stopping healthcare-associated infections (HAIs), and lengthening the lifespan of sensitive clinical tools. Throughout the surgical system, gadgets are exposed to tissues, physical fluids, and microbial contamination that must be completely removed in advance than reuse. Since even a small evidence of contamination can bring about extreme issues, hospitals need to adopt a scientific, genuine, thorough, and proof-based process for managing contraptions. Here is a complete, unique, complete, and sensible guide to well easy and keep surgical instruments to ensure the very best first-rate of hospital treatment.
Understanding the Importance of Proper Instrument Sterilization
Sterilization is extra than cleansing; it is important for controlling contamination. Instruments utilized in surgical procedure come into direct contact with inner tissues, implants, and the bloodstream. This means the hazard of blunders is virtually none. Instruments that are not nicely processed can deliver risky pathogens, including MRSA, E. Coli, Hepatitis viruses, and different microorganisms that thrive on surfaces.
Ensuring proper sterilization protects:
- Patients may be prevented from postoperative infections
- Healthcare employees in cutting down publicity to biohazards
- Facilities to help in regulatory compliance
- The sturdiness of the system is ensured through minimizing mechanical put on and corrosion
The strict sterilization process additionally guarantees that centers observe the requirements of groups which includes the CDC, WHO, ASTM, and AAMI.
Step 1: Pre-Cleaning — The Critical First Stage
The sterilization method starts offevolved at once after the units are used. Pre-cleansing prevents natural rely and organic materials from drying out and adhering to device surfaces.
Key Pre-Cleaning Steps:
- Clean up the gross waste with sterile water or an enzyme solution.
- Keep the units damp in a chosen transport field.
- Beware of the usage of saline, that can motive pitting and corrosion.
- Send the item quick to the decontamination place.
Pre-cleaning greatly improves the effectiveness of the sterilization and cleaning procedures by means of liberating bioburden before it becomes firmly bonded.
P 2: Thorough Cleaning and Decontamination
Cleaning eliminates micro- and visible debris, whilst decontamination lowers the microbial burden. Instruments can be cleaned with the aid of hand or with computerized instruments.
Manual Cleaning
- Use mild, authorized brushes and detergents.
- Instruments which might be easy and hinged within the open position.
- Avoid the use of abrasive pads or corrosive chemicals.
Ultrasonic Cleaning
This technique uses sound waves to cast off dust from hard-to-reach crevices, supplying more effective cleansing than conventional techniques by myself.
Washer-Disinfectors
The automatic structures clean and rinse contraptions, then thermally disinfect them, providing constantly reliable results.
Step 3: Inspection and Functional Testing
Before contraptions are sterilized, they need to be cautiously scrutinized for any harm, cleanliness, or mechanical problems. Even small imperfections can compromise the performance of surgical processes and the sterilization manner.
Inspection Checklist:
- Find cracks, pitting, or staining
- Check the sharpness of the scissors and cutting tools.
- Test hinges, ratchets, and needle holders
- Make positive that every one instruments with a lumen are clean of obstructions
Every tool that fails inspection need to be repaired or removed from circulate.
Step 4: Packaging for Sterilization
Proper packaging safeguards contraptions for the duration of the sterilization manner and guarantees sterility until use.
Best Practices:
- Utilize sterilization-grade wraps, pouches, or inflexible containers
- Unlock all hinges and lock
- Place the heavier gadgets at the decrease give up of the shelf.
- Be sure to preserve the steam moving freely
- Include chemical indicators in each %. Include chemical signs interior every
Correct packaging allows prevent infection and improve the performance of the sterilization system.
Step 5: Sterilization Methods Used in Medical Facilities
Different units require distinct sterilization tactics primarily based at the materials, thermal resistance, or even complexity.
1. Steam Sterilization (Autoclaving)
The most popular and most efficient method.
- Temperature: 121 °C- 134 °C
- Pressure: 15-30 psi
- Time for publicity: four-half-hour
Steam quick destroys the spores of micro organism and viruses. It is also less costly and secure for most chrome steel units.
2. Ethylene Oxide (ETO) Sterilization
For gadgets which can be touchy to heat.
- Low-temperature
- Permeates complicated lumens
- The method calls for an prolonged aeration to put off residual gasoline
3. Hydrogen Peroxide Plasma Sterilization
Perfect for heat- and sensitive instruments.
- Quick turnaround
- No harmful residues
- Not suitable for cellulose-primarily based materials.
4. Dry Heat Sterilization
Useful for oils, powders, and sharp gear.
5. Chemical (Cold) Sterilization
When heat-based techniques are not feasible, but, they require strict exposure intervals and careful handling.
Step 6: Safe Cooling and Post-Sterilization Handling
After sterilization is finished, the instruments have to cool in the sterilizer before managing. Hot packs could transfer bacteria into the packaging, compromising sterility.
Key Rules:
- Never cope with heat packs.
- Maintain devices which have been sterilized in a smooth place
- Inspect internal and external signs.
- Document consequences of the cycle
Proper handling will keep instruments clean until they are needed.
Step 7: Storage and Organization of Sterile Instruments
Storage areas ought to be maintained below ideal environmental conditions to make certain the units continue to be easy.
Proper Storage Conditions:
- Temperature: 18-24 °C
- Humidity: 35-70%
- Well-ventilated and dirt-free
- Shelves must be approximately eight inches faraway from the floor and a pair of inches far from the wall
Sterile resources should be organized by way of date to make sure first-in, first-out (FIFO) use.
Instrument Maintenance: Extending Lifespan and Performance
Maintenance prevents mechanical screw ups and guarantees gadgets perform easily.
Routine Maintenance Includes:
- Regularly lubricating joints the use of surgical-grade milk for instruments
- Regular sharpening of scissors is essential to make certain the slicing edges are sharp.
- Removal of rust, stains, or pitting
- Calibration assessments for sensitive equipment
Regular renovation can reduce fees via lowering the need for highly-priced maintenance or replacements.
Common Problems and How to Solve Them
1. Staining or Discoloration
Most often, the problem is because of low water satisfactory or incompatible detergents.
2. Rust or Corrosion
It happens while devices are uncovered to blood, saline, or irrelevant storage conditions.
3. Wet Packs
The purpose is normally due to overloading of the sterilizer, wrong drying, or insufficient wrapping.
4. Autoclave Malfunctions
It is important to troubleshoot and file the problem to keep away from reprocessing errors immediately.
Compliance and Documentation
Sterile processing companies should adhere to strict tips for documenting to stay in compliance with the regulatory organizations.
Required Records:
- Logs of the cycle of sterilization
- Reports on organic indicators
- Maintenance logs
- Employee competency statistics
Compliance guarantees felony safety and steady first-class assurance.
Conclusion
Proper sterilization and maintenance of surgical gadgets are critical to making sure the safety and effectiveness of clinical remedy. By following dependent approaches — pre-cleaning, unique washing, good enough inspection, appropriate packaging, and validated sterilization cycles — healthcare facilities dramatically lessen infection dangers and prolong the lifespan of critical surgical equipment. Each degree of the procedure plays a crucial role in ensuring affected person safety, attaining top-high-quality surgical consequences, and complying with regulatory authorities. If sterilization teams are properly skilled and cling to evidence-primarily based suggestions, they could create a manner that improves performance, safety, and the long-time period effectiveness of gadgets.
Read more on KulFiy
